Breast Care & Awareness
What is Breast Care & Awareness?
Breast care and awareness are critical aspects of women’s health, encompassing practices that support early detection and prevention of breast diseases, most notably breast cancer. By educating themselves and regularly performing breast self-examinations, women can significantly enhance their chances of detecting any changes early, leading to more effective treatment options if necessary.
Importance of Breast Awareness
Being breast-aware involves understanding the normal look and feel of your breasts. Changes to monitor include:
- Lumps or thickening in the breast or underarm area
- Changes in the size, shape, or contour of the breast
- Inverted nipples or changes in nipple appearance
- Redness, soreness, rash, or swelling
- Discharge other than breast milk, especially blood
- Persistent pain in a particular part of the breast or armpit
Breast Health
Breast health is a crucial aspect of women's healthcare. It focuses on maintaining and monitoring breast tissue to detect any abnormalities early. One of the primary methods for promoting breast health is breast self-examination (BSE).
What is Breast Self-Examination?
BSE is a very useful and important routine for women to perform regularly. This self-check can lead to early detection of lumps, changes, or abnormalities in breast tissue, which is crucial in the fight against breast cancer.
Importance of Breast Self-Examination
Breast self-examinations help individuals become familiar with the appearance and feel of their breasts. This familiarity makes it easier to notice any changes should they occur. While not all breast lumps or changes lead to breast cancer, early detection can play a pivotal role in providing more effective treatment options if the changes are indeed cancerous.
When to Perform a Breast Self-Examination?
Women can start practising breast self-exams from the age of 20 and continue throughout their lives, even after menopause.
If you still menstruate, the best time to do a breast self-exam is when your breasts are least likely to be tender or swollen, such as a few days after your period finishes. If you no longer menstruate, pick a certain day, such as the first day of each month, to remind yourself to do a breast self-exam.
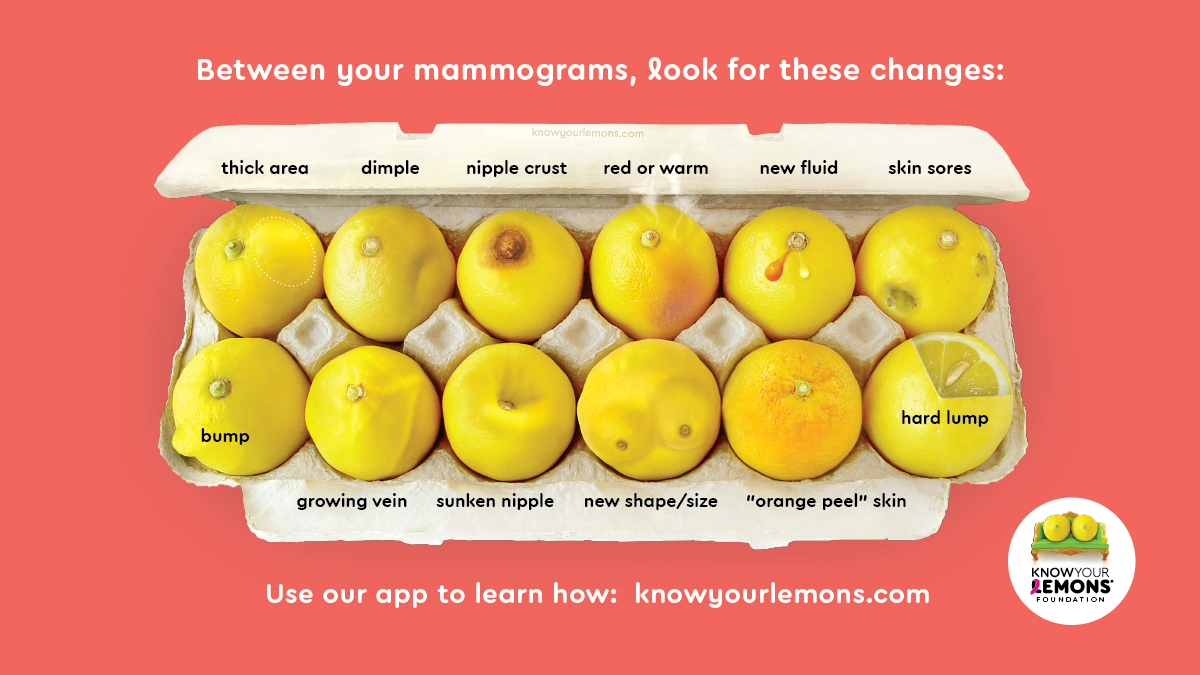
What Breast Changes To Look For?
Changes in the breasts may be warning signs of breast cancer. The Know Your Lemons diagram shows the 12 signs of breast cancer to look and feel for. All these changes can also have benign causes. If you notice changes that persist for 2 to 3 weeks, see your doctor without delay.
Guidelines for Breast Self-Examination
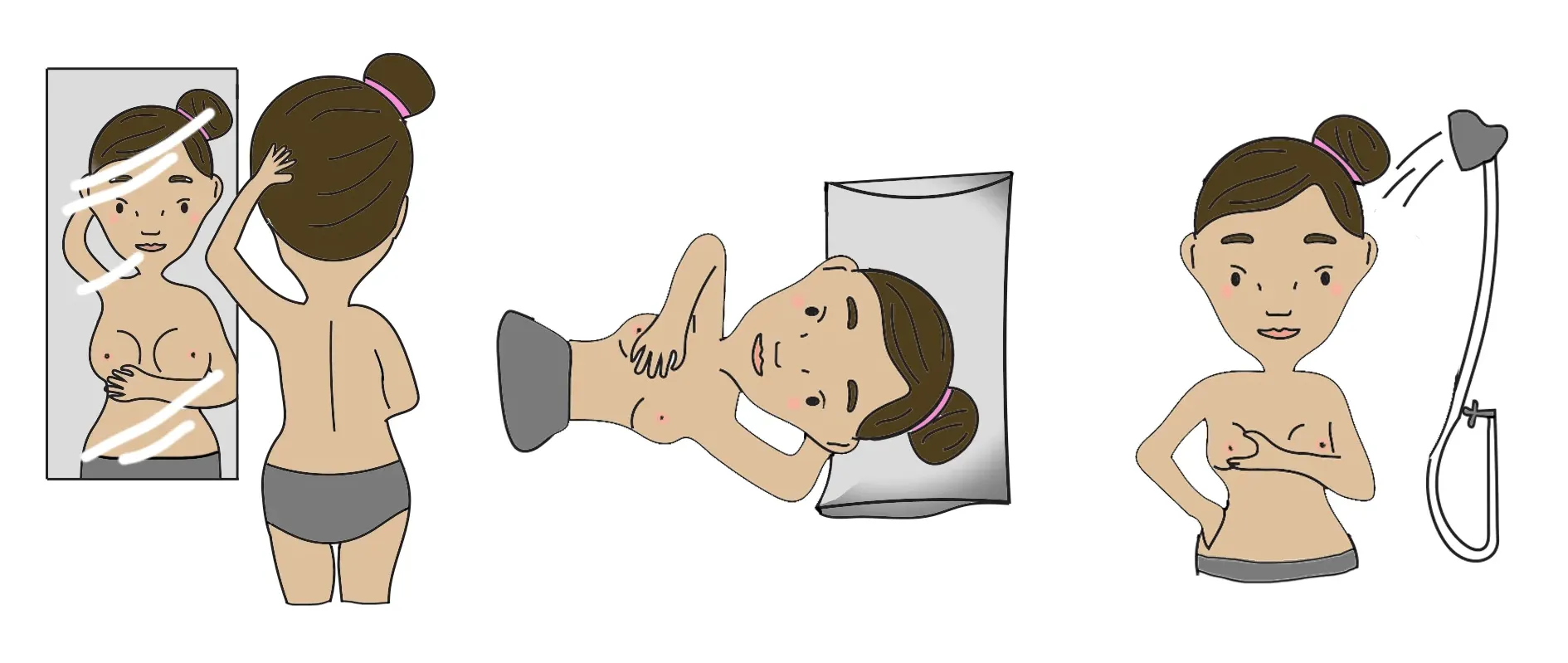
Breast self-examination should be performed once a month, ideally simultaneously each month. For menstruating women, the best time for BSE is a few days after the end of the menstrual period when the breasts are least likely to be swollen and tender. Here are general steps to follow:
- Visual Inspection: Stand in front of a mirror with straight shoulders and arms on your hips. Look for any changes in the contour, swelling, dimpling of the skin, or changes in the nipples. Then, raise your arms and look for the same changes.
- Physical Examination: Lie down and use your right hand to feel your left breast and vice versa. Use a firm, smooth touch with your hand's first few finger pads, keeping the fingers flat and together. Use a circular motion about the size of a quarter. Cover the entire breast from top to bottom, side to side—from your collarbone to the top of your abdomen and from your armpit to your cleavage.
- Examine Under Water: Many women find that the easiest way to feel their breasts is when their skin is wet and slippery, so they choose to do this part in the shower. Move your fingers in a similar pattern while examining each breast.
Additional Tips for Effective BSE
- Consistency: The key to breast self-examination is consistency. Perform it at the same time each month so that you can compare changes effectively.
- Record Keeping: It may help to keep a journal of your self-exams. This can help you remember what is normal for your breasts and what has changed if anything.
- Professional Evaluation: If you notice any unusual changes in your breasts during your self-examinations, consult a doctor as soon as possible. Do not panic, but do not ignore your findings either.
Professional Screenings
Apart from self-exams, clinical breast exams and mammograms are crucial. Guidelines suggest that women should have clinical breast exams every three years starting in their 20s and 30s and every year for women 40 and older. Mammography screening guidelines vary, but generally, women are advised to start regular mammography between the ages of 40 and 50.
Breast Changes Through the Menstrual Cycle
The menstrual cycle causes regular changes in hormone levels, particularly oestrogen and progesterone, which affect the breast tissues. These hormonal fluctuations can lead to:
- Swelling and Tenderness: Breasts may feel fuller and more sensitive or painful, especially in the days leading up to a period. This is due to oestrogen and progesterone enlarging the milk glands and ducts.
- Lumps: Some women experience fibrocystic breast changes, where lumpy areas or a general lumpiness in the breasts become more noticeable before menstruation. These lumps are benign and usually subside after the period begins.
- Texture Changes: The breasts may feel more granular or rope-like due to these hormonal changes.
These symptoms should resolve after the onset of menstruation, and familiarising oneself with these changes through regular breast self-examinations can help distinguish normal cyclical changes from unusual ones.
Breast Changes in Pregnancy and Breastfeeding
Pregnancy and breastfeeding bring about some of the most significant changes to the breasts as they prepare for milk production and feeding.
- Size Increase: Breasts often enlarge significantly during pregnancy due to increased blood flow, fat buildup, and the growth of milk-producing glands. This can continue during breastfeeding.
- Areola and Nipple Changes: The areolas may darken and enlarge, and nipples may become more pronounced, sensitive, or tender. Montgomery's glands around the nipples may also become more noticeable.
- Veins and Skin Changes: Due to increased blood supply, the skin of the breasts may stretch and show more visible veins.
- Colostrum Production: Late in pregnancy, breasts may start to produce colostrum, the first form of milk, which is thick and yellowish. During breastfeeding, breasts may become engorged, feel lumpy, and occasionally painful or prone to infections such as mastitis.
After breastfeeding, breasts may not return completely to their pre-pregnancy size or shape, as the tissues involved in milk production shrink back but might not be as firm as before.
Breast Changes in Menopause
As women enter menopause, oestrogen levels decline significantly, which affects breast tissue.
- Size and Firmness: Breasts may lose their fullness and firmness and appear saggy due to decreased glandular tissue and increased fatty tissue.
- Tenderness: Although less common than during the menstrual cycle, breasts can still become tender or sore during menopause, likely due to hormonal fluctuations.
- Lumps: Postmenopausal women may also experience benign breast lumps, such as cysts. However, any new breast lumps should be evaluated by a doctor as the risk of breast cancer increases with age.
Importance of Monitoring Changes
While most breast changes through these stages are normal, any new, unusual, or persistent changes should be discussed with a doctor. Regular breast self-examinations and awareness of one's own body play critical roles in identifying potential health issues early. Women should also continue routine screenings, such as mammograms, as doctors recommend based on their risk factors.
By understanding the normal patterns and changes in breast health related to life stages, women can better monitor their health and promptly address any concerns with their doctors. This knowledge empowers women to take proactive steps in managing their breast health effectively.